When Eye Inflammation Needs Careful Attention
Uveitis refers to inflammation inside the eye, affecting the uvea, the middle layer that includes the iris, ciliary body, and choroid. It can lead to redness, pain, light sensitivity, and vision changes. Sometimes it appears suddenly, while in other cases it develops slowly and becomes chronic.
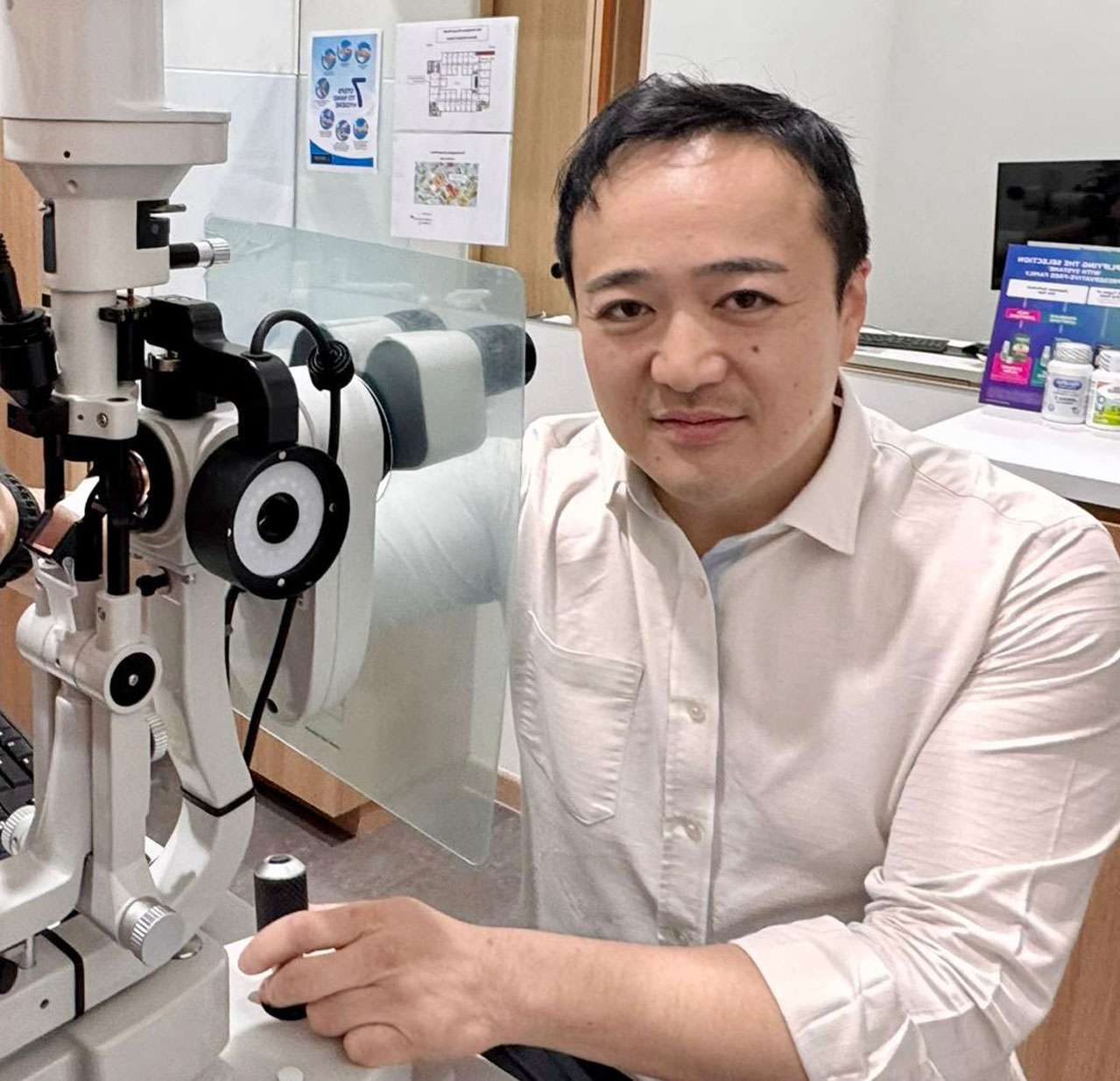
At London Eye & Retina, we provide thorough evaluation and long-term management of uveitis. Because it may be linked to underlying health conditions, a detailed, multidisciplinary approach is often needed.
What Is Uveitis?
Uveitis is not a single disease, but a group of inflammatory conditions affecting the eye’s internal structures. It may involve:
- Anterior uveitis – inflammation of the iris (most common)
- Intermediate uveitis – affecting the vitreous and peripheral retina
- Posterior uveitis – involving the retina or choroid
- Panuveitis – inflammation of all layers of the uvea
It can affect one or both eyes, and may recur over time.
What Causes Uveitis?
In many cases, the exact cause of uveitis is unknown. However, it may be linked to:
- Autoimmune or inflammatory diseases (e.g. ankylosing spondylitis, lupus, Behçet’s disease)
- Infections (e.g. tuberculosis, syphilis, toxoplasmosis, viral infections)
- Eye trauma or surgery
- Systemic infections or inflammatory syndromes
- Idiopathic (no identifiable cause)
Identifying the cause helps guide treatment and prevent complications.
What Are the Symptoms?
Uveitis symptoms can vary depending on the part of the eye affected. Common signs include:
- Eye redness
- Eye pain or discomfort
- Blurred or cloudy vision
- Light sensitivity (photophobia)
- Floaters (spots or shadows in vision)
- Decreased vision
- Tearing or watery eyes
Sudden onset or persistent symptoms should be assessed promptly, especially if they worsen over time.
How Is Uveitis Diagnosed?
A thorough eye examination is the first step. At London Eye & Retina, this may include:
- Slit-lamp examination to detect inflammation in the anterior chamber
- Dilated fundus examination to assess the retina and vitreous
- Optical Coherence Tomography (OCT) to monitor retinal or macular swelling
- Fundus photography to document inflammation
- B-scan ultrasonography (if the view to the back of the eye is obscured)
In some cases, additional tests such as blood work, chest imaging, or infectious disease screening may be needed. For unexplained or persistent uveitis, a vitrectomy biopsy may be considered.
Treatment Options
Treatment depends on the cause, location, and severity of inflammation:
- Topical steroid eye drops for anterior uveitis
- Oral or injectable steroids for intermediate or posterior uveitis
- Immunosuppressive medications or biologics for autoimmune-related uveitis
- Antibiotics or antivirals for infectious uveitis
- Surgical intervention (e.g. vitrectomy) in severe or non-responsive cases
Ongoing monitoring is key, as inflammation can recur or lead to complications such as glaucoma, cataracts, or macular edema.
Living with Uveitis
Chronic or recurrent uveitis can impact daily life, particularly if it affects vision or is linked to systemic health conditions. We aim to provide long-term support, helping you understand your condition and adjust treatment when needed.
Collaborative care with rheumatologists, infectious disease specialists, or internists may be recommended in complex cases.
When to See a Specialist
If you have recurrent red eyes, vision changes, or a known autoimmune condition with eye symptoms, don’t delay assessment. Early treatment can reduce the risk of long-term damage.
Book a consultation at London Eye & Retina for a comprehensive uveitis workup and personalised care plan.
Thoughtful Care for Complex Eye Conditions