Your Vision Matters, Especially When You Have Diabetes
Living with diabetes means keeping an eye on more than just your blood sugar. Over time, high blood sugar levels can damage the tiny blood vessels in the retina, leading to a group of eye problems collectively known as diabetic eye disease.
At London Eye & Retina, we believe that protecting your eyesight is an essential part of managing your diabetes. Through early detection, regular monitoring, and individualised care, we help patients stay ahead of vision complications.
What Is Diabetic Eye Disease?
Diabetic eye disease refers to a range of conditions that can affect individuals with Type 1 or Type 2 diabetes. These include:
- Diabetic Retinopathy – damage to the retinal blood vessels, which can leak fluid or bleed
- Diabetic Macular Edema (DME) – swelling in the macula, the part of the retina responsible for sharp central vision
- Cataracts – clouding of the eye’s lens, which can occur earlier in people with diabetes
- Glaucoma – increased pressure in the eye, potentially leading to optic nerve damage
Of these, diabetic retinopathy is the most common and a leading cause of vision loss in working-age adults worldwide.
Who Is at Risk?
Anyone with diabetes is at risk of developing diabetic eye disease. However, the risk increases with:
- Longer duration of diabetes
- Poor blood sugar control
- High blood pressure or cholesterol
- Smoking
- Pregnancy (in women with pre-existing diabetes)
Good control of diabetes and regular eye exams can reduce the likelihood of complications, especially if caught early.
What Are the Symptoms?
In the early stages, diabetic retinopathy may not cause any noticeable symptoms. That’s why regular screening is so important.
As the condition progresses, you may experience:
- Blurred or fluctuating vision
- Dark spots or floaters
- Difficulty seeing at night
- Vision that seems washed out or distorted
- Sudden loss of vision (in more advanced stages)
Symptoms often affect both eyes, and they may worsen without warning.
How Is It Diagnosed?
At London Eye & Retina, we use detailed imaging and diagnostic tools to detect even early signs of diabetic eye disease:
- Dilated eye examination – allows a clear view of the retina and blood vessels
- Optical Coherence Tomography (OCT) – scans the retina for swelling or abnormal changes
- Fluorescein Angiography – a dye test to detect leaking or blocked blood vessels
These tests help determine the stage and severity of diabetic retinopathy or macular edema and form the basis of your treatment plan.
How Is Diabetic Eye Disease Managed?
Treatment depends on the stage and type of eye involvement. In many cases, early changes can be monitored with regular eye exams and improved blood sugar control. When intervention is needed, options may include:
- Anti-VEGF injections to reduce macular swelling and slow new vessel growth
- Laser therapy to seal leaking blood vessels or shrink abnormal ones
- Vitrectomy surgery for bleeding or severe scar tissue in advanced cases
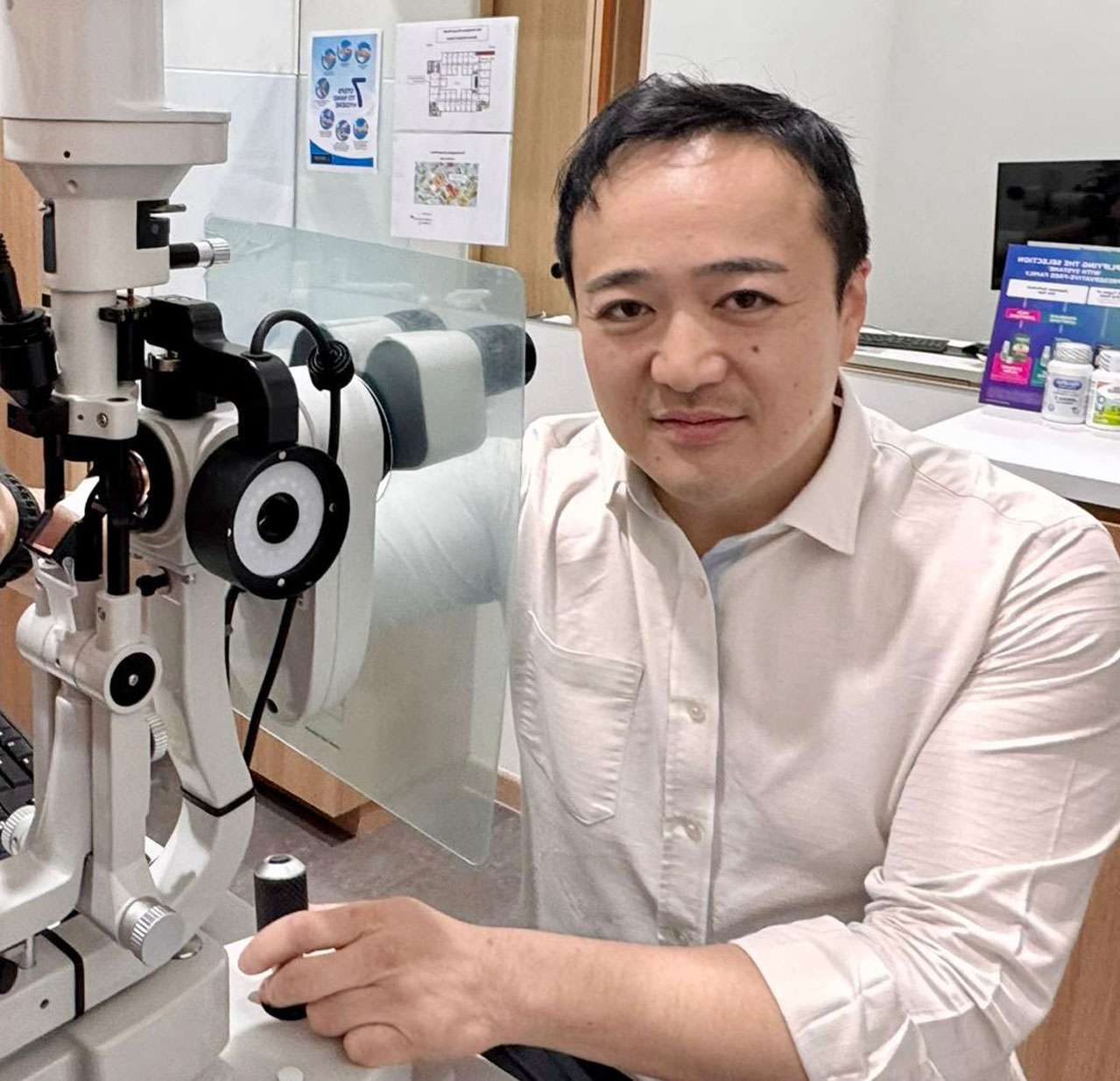
Dr James Ng will work with you to recommend an evidence-based approach that fits your condition and lifestyle. Our goal is to preserve vision while keeping your care plan as seamless and comfortable as possible.
Why Regular Screening Matters
Because early diabetic eye disease often has no symptoms, annual retinal exams are key, even if your vision seems fine. Timely detection can prevent or slow down progression and reduce the risk of vision loss.
Take the Next Step for Your Eyes
If you have diabetes, keeping your eyes healthy is not optional, it’s essential. Whether you’re newly diagnosed or have been managing diabetes for years, we’re here to support your eye health journey.
Book an eye screening at London Eye & Retina today. Early action can make all the difference.
Retinal Care for People Living with Diabetes